
Stroke risk factors you can't control
Factors outside your control can raise your risk of stroke. Learn what you can do to offset that risk.

Prior stroke
Having already had a stroke is the biggest risk factor for having another stroke. Read more.

Family health history
This does not mean that you will have a stroke too. But you may be more at risk if one of your parents had a stroke. Read more.

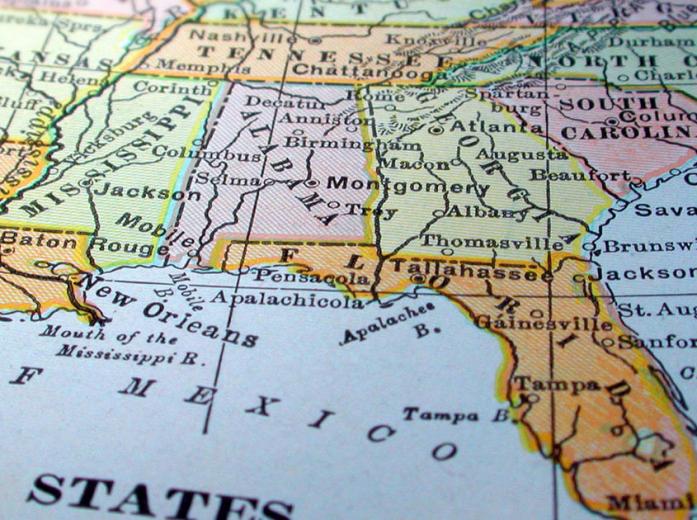
Where you live
You are more likely to have a stroke than other Americans if you are from one of the Southeastern states in the "Stroke Belt."5


Pregnancy history
High blood pressure or diabetes during pregnancy can raise your risk of stroke later in life. Read more.

Migraines
Having a migraine with aura raises your risk of stroke, especially if you are younger than 55. Read more.
Age and menopause
As a woman ages, her risk of stroke goes up each year by 10%.1
- When you are younger, your arteries have smooth linings and flexible walls that allow blood to flow freely. As you age, the linings get stiff and the walls thicken, which can make it harder for blood to flow. This is mainly caused by plaque buildup in your arteries, a process called atherosclerosis. Atherosclerosis begins in childhood.2 The older you are, the more likely your arteries will be narrowed or blocked enough to cause problems.
- Your chance of surviving a stroke also goes down as you get older. This is usually because you are more likely to have other health problems when you are older, such as high blood pressure, high cholesterol, or diabetes. These health conditions make it harder for your body to recover from stroke.
- Menopause raises your risk of stroke because your ovaries stop making estrogen. Estrogen is a hormone that may help keep blood vessels relaxed and open and help the body maintain a healthy balance of good and bad cholesterol. Without estrogen, cholesterol may start building up on artery walls. This can lead to stroke and other types of heart disease.
Menopausal hormone therapy
Many women take menopausal hormone therapy to help relieve menopause symptoms such as hot flashes. Results from a large study called the Women's Health Initiative showed that women taking menopausal hormone therapy with estrogen plus progesterone had a higher risk of stroke, serious blood clots, heart attacks, and other serious health problems. The risks were found to be much higher for women 60 years and older.
If you decide to use menopausal hormone therapy, talk to your doctor. The Food and Drug Administration advises women who want to try menopausal hormone therapy to use the lowest dose that works for the shortest time needed.
Read more about menopausal symptoms and hormone therapy in our Menopause section.
Personal and family health history
Having already had a stroke is the biggest risk factor for having another stroke.
Your family history also puts you at risk of a stroke. Your risk of stroke is higher if one of your parents, especially your mother, had a stroke.3,4
If stroke runs in your family, it may be because your family carries genes that raise your risk. An example would be a gene that makes your blood more likely to clot. Talk to your doctor about your family health history.
Race and ethnicity
Women who are black and non-Hispanic are more likely to have a stroke and die from stroke than white women.5 The reason for this is not totally clear. It is partly because many of the other risk factors for stroke are more common in black women than white women, including diabetes, obesity, high blood pressure, and high cholesterol. Black women are also less likely to get to the hospital in time for treatment with tPA, a clot-busting drug that must be given within 3 to 4½ hours of symptoms starting. Black women are also less likely to be treated with tPA if they do get to the hospital in time.
Some of these risk factors are also more common among women who are American Indian/Alaska Native and Hispanic. No matter your racial or ethnic group, you can take the same steps as any other woman to control your risk factors for stroke.
Pregnancy
During and soon after pregnancy, your risk of stroke is higher. Although pregnancy-related stroke is not common, the number of women who have a stroke during or soon after pregnancy is going up.7,8 This is likely because more women have other risk factors for stroke, including heart disease, overweight and obesity, and high blood pressure, during pregnancy.
The increased risk of stroke during pregnancy comes from several changes that happen to your body during pregnancy, such as increased blood clotting. Your body also makes more blood during pregnancy. After birth, these changes reverse rapidly, and this can trigger a stroke.
Some women are more at risk of pregnancy-related stroke. You may be more at risk if you already have risk factors for stroke, such as high blood pressure, and you:9
- Are African-American
- Are older than 35
- Have lupus
- Have migraine headaches
The best way to lower the risk of stroke during pregnancy is to control your stroke risk factors before you get pregnant.
Pregnancy history
Some health problems can happen during pregnancy and raise your risk of stroke later in life:
- Preeclampsia. Preeclampsia is a health problem that can happen during pregnancy. It is unexpected high blood pressure and problems with your kidneys (called "protein in the urine"). If you have ever had preeclampsia, you are at a higher risk of stroke even decades later. Having preeclampsia before 32 weeks of pregnancy is especially risky. This may be because women who get preeclampsia have other problems with their blood vessels that can also lead to stroke. Another reason could be that preeclampsia causes long-term changes in the blood vessels. If you've had preeclampsia, you are more likely to develop high blood pressure later in life, the number one stroke risk factor.
- Gestational high blood pressure (sometimes called gestational hypertension). High blood pressure during pregnancy can happen in some women who do not normally have high blood pressure. Gestational high blood pressure goes away after birth but raises your risk of stroke later in life, after pregnancy is over. Gestational high blood pressure can also lead to preeclampsia.
- Gestational diabetes. Having gestational diabetes (diabetes during pregnancy) puts you at higher risk of having type 2 diabetes later in life, after pregnancy is over. Diabetes is a major risk factor for stroke.
Learn more about these pregnancy complications in our Pregnancy section.
Migraine headaches
Having a migraine with aura (seeing bright flashing lights or spots that aren't real) raises your risk of stroke, especially if you are younger than 55 or if you smoke. Women on hormonal birth control pills who have migraine with aura are also at risk of stroke.10 Researchers are studying whether migraine raises stroke risk for women on other forms of hormonal birth control, like the patch or ring.
However, the overall risk of stroke for otherwise healthy women who get migraine is still low. The type of stroke that happens most often in women with migraine is also less serious. If you have migraine, talk to your doctor about your stroke risk.
Read more about migraine on our Migraine page.
Sources
- Asplund, K., Karvanen, J., Giampaoli, S., Jousilahti, P., Niemelä, M., Broda, G., … Kulathinal, S. (2009). Relative risks for stroke by age, sex, and population based on follow-up of 18 European populations in the MORGAM Project. Stroke, 40(7), 2319–2326.
- McGill, H. C., McMahan, C. A., Herderick, E. E., Malcolm, G. T., Tracy, R. E., & Strong, J. P. (2000). Origin of atherosclerosis in childhood and adolescence. American Society for Clinical Nutrition, 72(5), 1307s–1315s.
- Banerjee, A. A., Lim, C. C., Silver, L. E., Welch, S. J., Banning, A. P., & Rothwell, P. M. (2011). Familial History of Stroke Is Associated with Acute Coronary Syndromes in Women. Circulation: Cardiovascular Genetics, 4(1), 9–15.
- Goldstein, L. B., Adams, R., Becker, K., Furberg, C. D., Gorelick, P. B., Hademenos, G., … del Zoppo, G. J. (2001). Primary prevention of ischemic stroke: a statement for healthcare professionals from the Stroke Council of the American Heart Association. Stroke, 32, 280–299.
- Benjamin, E. J., Virani, S. S., Callaway, C. W., Chamberlain, A. M., Chang, A. R., Cheng, S., … Muntner, P. (2018). Heart Disease and Stroke Statistics—2018 Update: A Report From the American Heart Association. Circulation, 137, e67–e492.
- Bushnell, C., McCullough, L. D., Awad, I. A., Chireau, M. V., Fedder, W. N., Furie, K. L., … Walters, M. R. (2014). Guidelines for the Prevention of Stroke in Women. Stroke, 45.
- Berends, A. L., de Groot, C. J., Sijbrands, E. J., Sie, M. P., Benneheij, S. H., Pal, R., … Steegers, E. A. (2008). Shared constitutional risks for maternal vascular-related pregnancy complications and future cardiovascular disease. Hypertension, 51, 1034–1041.
- James, A. H., Bushnell, C. D., Jamison, M. G., & Myers, E. R. (2005). Incidence and risk factors for stroke in pregnancy and the puerperium. Obstetrics and Gynecology, 106(3), 509–516.
- Sacco, S., Ricci, S., Degan, D., & Carolei, A. (2012). Migraine in women: the role of hormones and their impact on vascular diseases. The Journal of Headache and Pain, 13(3), 177–189.


